BMR & TDEE Calculator
Calculate your Basal Metabolic Rate and Total Daily Energy Expenditure
Your Results
Understanding how many calories your body needs each day is foundational to nutrition, weight management, athletic performance, and public health planning. A bmr and tdee calculator is the practical tool that translates physiology into actionable numbers: basal metabolic rate (BMR) for resting energy needs and total daily energy expenditure (TDEE) for the calories you burn through living, working, and exercising. This long-form guide explains what those calculators measure, the science behind them, how to use them correctly, their historical development, comparisons of formulas, implementation in healthcare and community programs, regional and state-level impacts, success stories, common challenges, and future prospects. Throughout, you’ll find in-depth analysis, practical examples, and a FAQs section to help you confidently use a bmr and tdee calculator for personal or programmatic goals.
What are BMR and TDEE?
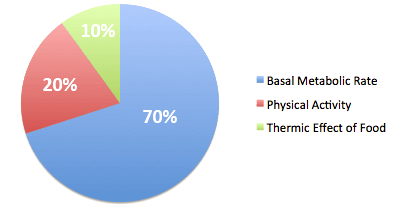
Basal Metabolic Rate (BMR) is the number of calories your body needs to maintain essential physiological functions—breathing, circulation, cell production—while at complete rest. Total Daily Energy Expenditure (TDEE) is BMR adjusted for your physical activity level and the energy used to digest food. A bmr and tdee calculator takes inputs like age, sex, height, weight, and activity level and produces estimates for both metrics so you can plan diets, set weight-loss or weight-gain goals, and tailor training.
A high-quality bmr and tdee calculator helps you move beyond guesswork to evidence-based planning. Whether the goal is sustainable weight loss, sports performance, or clinical nutrition management, the numbers from a bmr and tdee calculator provide a starting point for personalized plans.
Why energy calculators matter: objectives and practical uses
Medical professionals, fitness coaches, and public health practitioners use a bmr and tdee calculator to:
- Establish calorie targets for weight management programs.
- Adjust nutritional prescriptions for patients with metabolic disorders.
- Design training nutrition for athletes to match energy requirements.
- Inform community-level interventions addressing undernutrition or obesity.
- Evaluate program impacts in state-level health initiatives.
Accurate use of a bmr and tdee calculator supports individualized care and scaled policy interventions by converting clinical concepts into measurable, monitorable targets.
A brief history of metabolic calculators
The scientific quest to quantify human energy needs began in the late 19th and early 20th centuries with calorimetry experiments. Classic equations evolved over time:
- Early calorimetric work measured resting energy in controlled lab settings.
- The Harris-Benedict equations (1918) were among the first widely used predictive formulas.
- Later revisions and alternatives—Mifflin-St Jeor (1990), Katch-McArdle (lean-mass focused)—refined accuracy for varying populations.
Modern bmr and tdee calculator tools combine these formulas with standardized activity multipliers to estimate daily needs. Technological advances have moved calculators from pen-and-paper equations to mobile apps, websites, and electronic medical records, increasing accessibility for both individuals and public programs.
How a bmr and tdee calculator works (formulas and inputs)
A bmr and tdee calculator typically asks for:
- Age
- Sex
- Height
- Weight
- Activity level (sedentary, lightly active, moderately active, very active, extra active)
- Optionally: body fat percentage (for lean-mass–based calculations)
Common formulas used inside a bmr and tdee calculator:
- Harris-Benedict (revised) — widely available, historically influential.
- Mifflin-St Jeor — often considered more accurate for modern populations.
- Katch-McArdle — uses lean body mass when body-fat data are available.
Once BMR is computed by a bmr and tdee calculator, it multiplies BMR by an activity factor to estimate TDEE. For instance, a sedentary multiplier might be 1.2 while a very active multiplier might be 1.725; a bmr and tdee calculator uses these to produce practical calorie targets.
Step-by-step: using a bmr and tdee calculator correctly
- Enter accurate anthropometrics: use your most recent weight and measured height.
- Choose the formula that matches your context: if you know body-fat percentage, use Katch-McArdle within your bmr and tdee calculator.
- Be honest about activity level: overestimating activity will overstate calorie needs.
- Use the TDEE result as a baseline, not an immutable destiny—monitor outcomes and adjust.
- Recalculate after significant weight or activity changes; a bmr and tdee calculator can and should be reused as you progress.
A bmr and tdee calculator is only as good as the inputs and the ongoing feedback loop you create with monitoring, adjustments, and professional oversight when needed.
Formulas explained: Harris-Benedict, Mifflin-St Jeor, and Katch-McArdle
A typical bmr and tdee calculator offers formula choices; understanding their strengths helps you choose.
- Harris-Benedict (revised): uses weight, height, age, sex. Historically prevalent, it can overestimate BMR in modern sedentary populations.
- Mifflin-St Jeor: developed later, often considered more accurate for present-day adults and frequently preferred in a bmr and tdee calculator.
- Katch-McArdle: calculates BMR from lean body mass, ideal when body composition data are available.
Different bmr and tdee calculator results reflect population diversity. Clinicians working with elderly, pediatric, or clinical populations should exercise care and may use indirect calorimetry where possible.
Sample calculation: from data to daily calories
Consider a 35-year-old woman, 165 cm, 70 kg, lightly active. A bmr and tdee calculator using Mifflin-St Jeor might produce:
- BMR ≈ (10 × 70) + (6.25 × 165) − (5 × 35) − 161 = 1,430 kcal (approx).
- Activity multiplier (light) = 1.375 → TDEE ≈ 1,430 × 1.375 ≈ 1,966 kcal/day.
A bmr and tdee calculator presents this as a baseline; to lose weight, a typical recommendation would subtract 300–500 kcal/day carefully under guidance. This concrete example shows how a bmr and tdee calculator clarifies the math behind dietary plans.
Accuracy and limitations of a bmr and tdee calculator
No predictive model is perfect. Limitations include:
- Population bias: Many formulas were developed on specific cohorts and may misestimate in other ethnic or regional groups.
- Self-reported activity: Users often overestimate physical activity levels.
- Composition sensitivity: Two people with identical weight may have different metabolisms depending on lean mass; a bmr and tdee calculator that lacks body-composition input will miss that nuance.
Despite limits, a bmr and tdee calculator remains a powerful starting point if used with iterative monitoring and adjustments.
Clinical and public-health implementation: programs and policy framework
A bmr and tdee calculator is not only a tool for individuals but also an instrument in broader programs. Integrating these calculators into health services supports:
- Nutritional counseling in primary care.
- Tailored interventions in maternal and child health programs.
- Workforce wellness and chronic disease prevention initiatives.
From a policy framework viewpoint, deploying standardized bmr and tdee calculator tools can help governments monitor population-level nutritional status, design targeted campaigns for women empowerment schemes focused on nutritional education, and allocate resources to rural development programs where undernutrition remains prevalent. A bmr and tdee calculator thus becomes intertwined with social welfare initiatives aimed at improving health outcomes.
State-wise benefits and regional impact
When state health departments incorporate a bmr and tdee calculator into public programs, benefits include:
- Data-driven allocation of nutrition supplements and counseling resources.
- Customization of community programs to local activity patterns and occupational demands.
- Enhanced targeting of vulnerable populations in state-wide women empowerment schemes or rural development projects by identifying calorie deficits or excesses.
Successful state-level rollouts of digital bmr and tdee calculator tools can reveal regional disparities—urban centers may show overnutrition trends while rural areas still struggle with undernutrition—informing policy shifts and resource reallocation.
Case studies and success stories
Several hypothetical and real-world implementations demonstrate the value of integrating a bmr and tdee calculator into programmatic settings:
- Community health workers using a simple bmr and tdee calculator in a rural outreach program to create personalized counseling plans for mothers, leading to improved maternal BMI and infant growth indices.
- A workplace wellness initiative that provided employees with individualized TDEE reports and saw collective improvements in physical activity and reductions in sick leave.
- An athletic training center employing a precise bmr and tdee calculator tied to body-composition analysis to optimize athletes’ fueling strategies and boost performance outcomes.
These success stories show the practical benefits of translating numbers from a bmr and tdee calculator into sustained behavior change and measurable outcomes.
Challenges in scale and equity
Scaling a bmr and tdee calculator across diverse regions and populations faces challenges:
- Digital access: rural communities may lack reliable internet or devices to access online calculators.
- Cultural relevance: dietary norms and activity patterns vary; calculators must be contextualized.
- Data privacy: storing anthropometric and health data requires secure systems to protect participants.
- Literacy and numeracy: users may need support interpreting a bmr and tdee calculator output.
Addressing these challenges requires integrating calculators into human-centered delivery models—training community health workers, ensuring offline tool availability, and aligning tools with local languages and customs.
Comparison with other nutritional tools and schemes
A bmr and tdee calculator differs from other nutritional tools and public schemes in key ways:
- Compared with simple BMI screening, a bmr and tdee calculator provides dynamic energy targets rather than a static risk label.
- Nutritional supplementation schemes often distribute calories uniformly; a bmr and tdee calculator enables personalization to individual or household needs.
- Compared with large-scale fortification programs, a bmr and tdee calculator focuses on behavioral change and personalized targets rather than broad population-level micronutrient delivery.
In program design, combining a bmr and tdee calculator with other interventions—food fortification, policy-level food subsidies, and social welfare initiatives—creates more holistic strategies to tackle both undernutrition and obesity.
Integrating a bmr and tdee calculator into women empowerment schemes
Empowerment programs that include nutrition literacy modules benefit from integrating a bmr and tdee calculator because:
- Women, especially mothers and caregivers, can use personalized calorie targets to improve household nutrition.
- Nutrition education combined with individualized calculators supports informed decision-making on food allocation and meal planning.
- When tied to income-generation or microcredit initiatives, a bmr and tdee calculator can help participants budget for nutrient-dense foods and monitor outcomes.
Embedding such calculators into training sessions enhances the program’s capacity-building objectives and encourages long-term behavioral change.
Rural development and community nutrition
Rural development programs addressing food security and livelihoods can leverage a bmr and tdee calculator in several ways:
- Assess occupational energy needs: agricultural laborers expend more energy; a bmr and tdee calculator helps set higher calorie benchmarks for such populations.
- Design food support: targeted rations can be adjusted based on TDEE outputs rather than a one-size-fits-all approach.
- Monitor program impact: repeated measurements using a bmr and tdee calculator over time provide localized data on nutritional status changes.
A rural development strategy that uses bmr and tdee calculator evidence can align food production, market access, and health interventions for maximum nutritional benefit.
Data-driven social welfare initiatives
Social welfare initiatives that incorporate a bmr and tdee calculator can improve targeting and accountability:
- Conditional cash transfers tied to maternal and child nutrition benchmarks assessed via calculators can ensure benefits support health goals.
- Community nutrition centers using standardized calculators can aggregate anonymized data to inform policy decisions across districts and states.
- Integrating bmr and tdee calculator outputs into monitoring frameworks strengthens evidence-based policymaking.
By treating the calculator as a measurement instrument within larger monitoring systems, policymakers can better evaluate program efficacy and adjust strategies.
Technology and user experience: designing an effective bmr and tdee calculator
A user-friendly bmr and tdee calculator should feature:
- Clear input fields and guidance on how to measure weight and height.
- Multiple formula options with explanations for each choice (Harris-Benedict, Mifflin-St Jeor, Katch-McArdle).
- Localized units (kg/cm and lb/in) and language support.
- Offline functionality for low-connectivity environments.
- Data privacy assurances and optional exportable reports for healthcare providers.
Thoughtful UI/UX design increases uptake and ensures a calculator is accessible to diverse users, from young athletes to community health workers.
Ethical considerations and data privacy
Collecting health data via a tdee calculator raises ethical obligations:
- Secure storage and minimal data retention periods safeguard users.
- Transparent consent processes—especially for minors and vulnerable groups—are critical.
- Ensuring calculators do not exacerbate body-image issues or disordered eating behaviors requires careful framing and professional linkage.
Governance frameworks and provider training reduce ethical risks when deploying a bmr and tdee calculator at scale.
Monitoring and evaluation: measuring impact
To evaluate the effectiveness of interventions using a calculator, programs should:
- Establish baseline measurements and follow-up intervals.
- Use standardized protocols for data collection and interpretation.
- Combine calculator outputs with anthropometric measures and qualitative feedback.
- Report disaggregated results by age, sex, and region to detect inequities.
Robust evaluation turns a calculator from a diagnostic tool into a lever for continuous improvement.
Comparisons with direct measurement: when to use indirect vs. direct methods
Indirect methods (predictive equations in a bmr and tdee calculator) are practical and cost-effective. Direct methods—indirect calorimetry for BMR or doubly labeled water for TDEE—are more accurate but expensive and less scalable. Programs should reserve direct measures for research, high-stakes clinical decisions, or validation studies, while using a bmr and tdee calculator for routine clinical practice and program delivery.
Training and capacity building
Scaling a calculator requires capacity building among:
- Primary-care clinicians to interpret results and prescribe nutrition plans.
- Community health workers to collect reliable inputs and provide counseling.
- Program managers to integrate outputs into workflows and reporting systems.
Training ensures consistent use of calculators and reduces variability in counseling quality.
Barriers to adoption and how to overcome them
Common barriers include lack of trust in digital tools, low numeracy, and cultural resistance. Solutions:
- Pair calculators with in-person counseling to explain results.
- Provide visual and plain-language explanations of what BMR and TDEE mean.
- Localize tools into regional languages and adapt activity multipliers to local occupations.
Bridging technical outputs from a bmr and tdee calculator with human support increases adoption and impact.
Future prospects: personalization, AI, and integration
The next generation of calculator tools will likely integrate:
- Wearable data (heart rate, accelerometry) for dynamic TDEE estimation.
- Machine learning models that adapt formulas to local population data.
- Interoperability with electronic health records to track longitudinal changes.
- Behavior-change nudges tailored to individual context based on TDEE results.
These advances make a calculator not just a static estimator but a personalized, adaptive coach.
Policy recommendations for scaling up
To successfully integrate a bmr and tdee calculator into public health and welfare systems, policymakers should:
- Standardize validated formulas across programs while allowing local calibration.
- Invest in digital infrastructure and offline-capable tools for rural areas.
- Incorporate calculators into nutrition education in schools and community centers.
- Ensure data governance and privacy protections align with legal frameworks.
- Pilot inclusive programs that combine calculators with food security and women empowerment measures.
Policy alignment ensures that a calculator contributes meaningfully to health system goals.
Practical tips for individuals using a bmr and tdee calculator
- Recalculate every 4–8 weeks during weight-change phases.
- Use the calculator as a guideline and track actual intake and weight to refine plans.
- Combine calorie targets with macronutrient planning for satiety and performance.
- Consult a registered dietitian or physician if you have medical conditions before making major calorie changes.
A bmr and tdee calculator empowers individuals to make informed choices but should be used as part of a monitored, evidence-based approach.
Comparative summary: when to choose which formula
- Use Mifflin-St Jeor as the standard default in a bmr and tdee calculator for adult populations.
- Use Katch-McArdle if you have reliable body-fat percentage data.
- Consider Harris-Benedict for historical comparison or when using calculators that default to it.
Choosing the right formula in a calculator improves relevance and reduces systematic error.
Conclusion: the calculator as a bridge between science and practice
A bmr and tdee calculator translates physiological science into tangible, actionable daily targets. Whether used by an individual planning a weight-loss journey, a coach designing training nutrition, or a state health department tailoring nutrition programs, the calculator serves as a measurement and planning tool. Its greatest value comes when combined with monitoring, human support, ethical data practices, and integration into broader social welfare initiatives like women empowerment schemes and rural development programs. With better data, thoughtful implementation, and technological innovation, the bmr and tdee calculator will play an ever more central role in personalized nutrition and population health.